Dangers of Masks
Links regarding mask failures:
Mask Outcomes
https://thefederalist.com/2020/10/12/cdc-study-finds-overwhelming-majority-of-people-getting-coronavirus-wore-masks/
Let's take a brief journey into the success (or lack thereof) of masks in preventing the spread of coronavirus.
Come with me on a tour of the wonderful world of mask mandates and their results.
Here is a preview of our journey.
(1/16) pic.twitter.com/QKb8HUi1u9
— Yinon Weiss (@yinonw) October 27, 2020
Dangers of Lockdowns
New JAMA paper shows how lockdowns lead to more deaths:
"substantial decrease in the number of non–COVID hospitalizations for exacerbations of chronic conditions (heart failure, COPD), and acute medical events (myocardial infarction, appendicitis)."https://t.co/Aucjh1Hmji pic.twitter.com/DVBXKEnwgC
— Dr. Eli David (@DrEliDavid) October 28, 2020
Other Links
BREAKING: Danish mask study that JAMA, NEJM & Lancet REFUSED to publish was just published in Annals of Internal Medicine.
In the largest randomized controlled trial to date w/ 6,024 subjects, medical masks were NOT effective protection against infection.https://t.co/HyFiQX2qPG
— James Todaro, MD (@JamesTodaroMD) November 18, 2020
A massive Danish study on mask usage found no statistically significant difference in coronavirus infection rates between mask-wearers and non-mask-wearers. In fact, according to the data, mask usage may actually increase the likelihood of infection. https://t.co/ijUy8hfNTY pic.twitter.com/gYDtA8ac0p
— Sean Davis (@seanmdav) November 18, 2020
Maine’s Rise in COVID-19 Cases Linked to Face Masks; The Data Shows Prolonged Face Mask Use Increases Risk of Catching Respiratory Illness.
Chew on this Dr. Tam. Tamhttps://t.co/kUGxiX7iWs— Rocco Galati (@roccogalatilaw) November 15, 2020
2 mins research shows masks DO NOT WORK. And can lead to serious health problems like Hypoxia from wearing. How many studies and Doctors telling you this does it take for you to make an informed decision? This Doctor explains. Full vid here : https://t.co/rAImc3HoF7 pic.twitter.com/588fBDFMP0
— FFAC 🇨🇦 (@stevelanebitch) November 8, 2020
A must watch-clear talk. Dr mike Yeadon debunks the Covid Crisis with clear statements. The PCR test is unreliable, hospitalizations & deaths based on the PCR tests are misstated. Canada & Ontario are using the same falsehoods as the UK. To promote a falsehood today. #onpoli https://t.co/7I6CkdWTox
— Randy Hillier (@randyhillier) November 5, 2020
According to the Danish newspaper @berlingske tre scientific journals have refused to publish the results of the first major scientific investigation the effect of use of masks during the Covid-19 pandemic. Apparently because the results might not show what is politically correct pic.twitter.com/OJ6ZRq8idp
— Lars Christensen (@MaMoMVPY) October 21, 2020
Statment of claim – Violates our Charter rights
https://vaccinechoicecanada.com/wp-content/uploads/vcc-statement-of-claim-2020-redacted.pdf
Bad Fit for risk reduction
https://www.cmaj.ca/content/188/8/606
WHO on Masks
https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/q-a-on-covid-19-and-masks
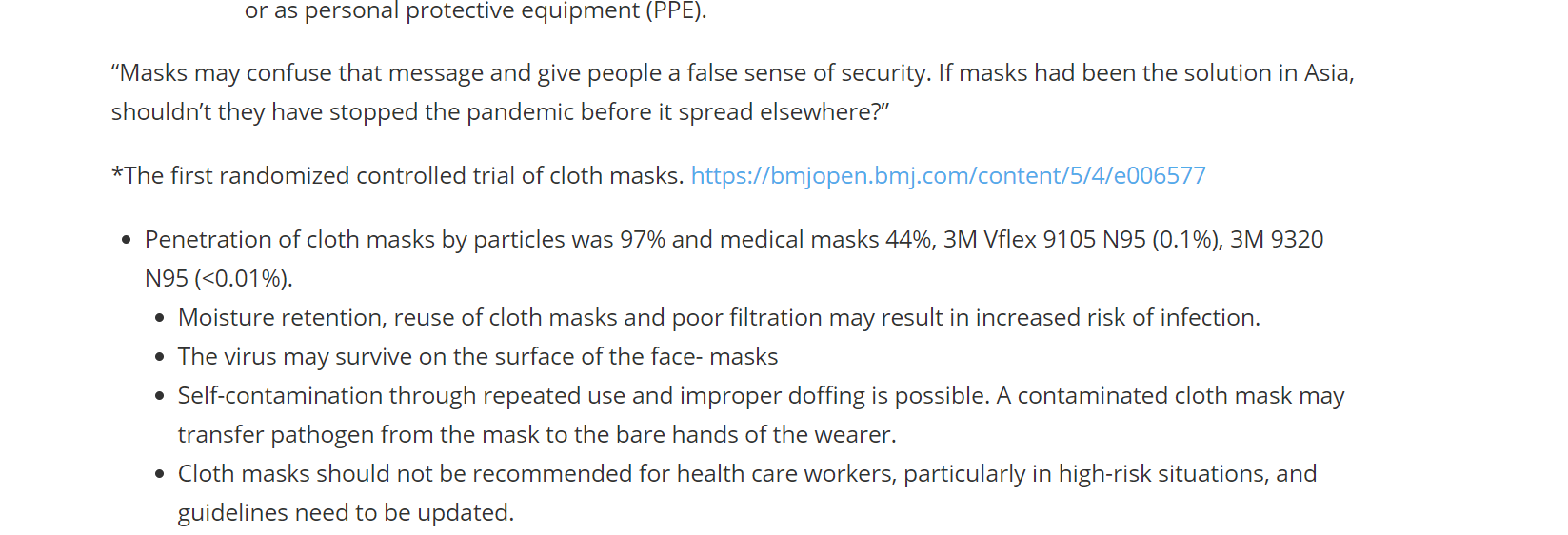
Masks hurt they don’t help
https://bmjopen.bmj.com/content/5/4/e006577
Masks for all not based on sound data
https://www.cidrap.umn.edu/news-perspective/2020/04/commentary-masks-all-covid-19-not-based-sound-data
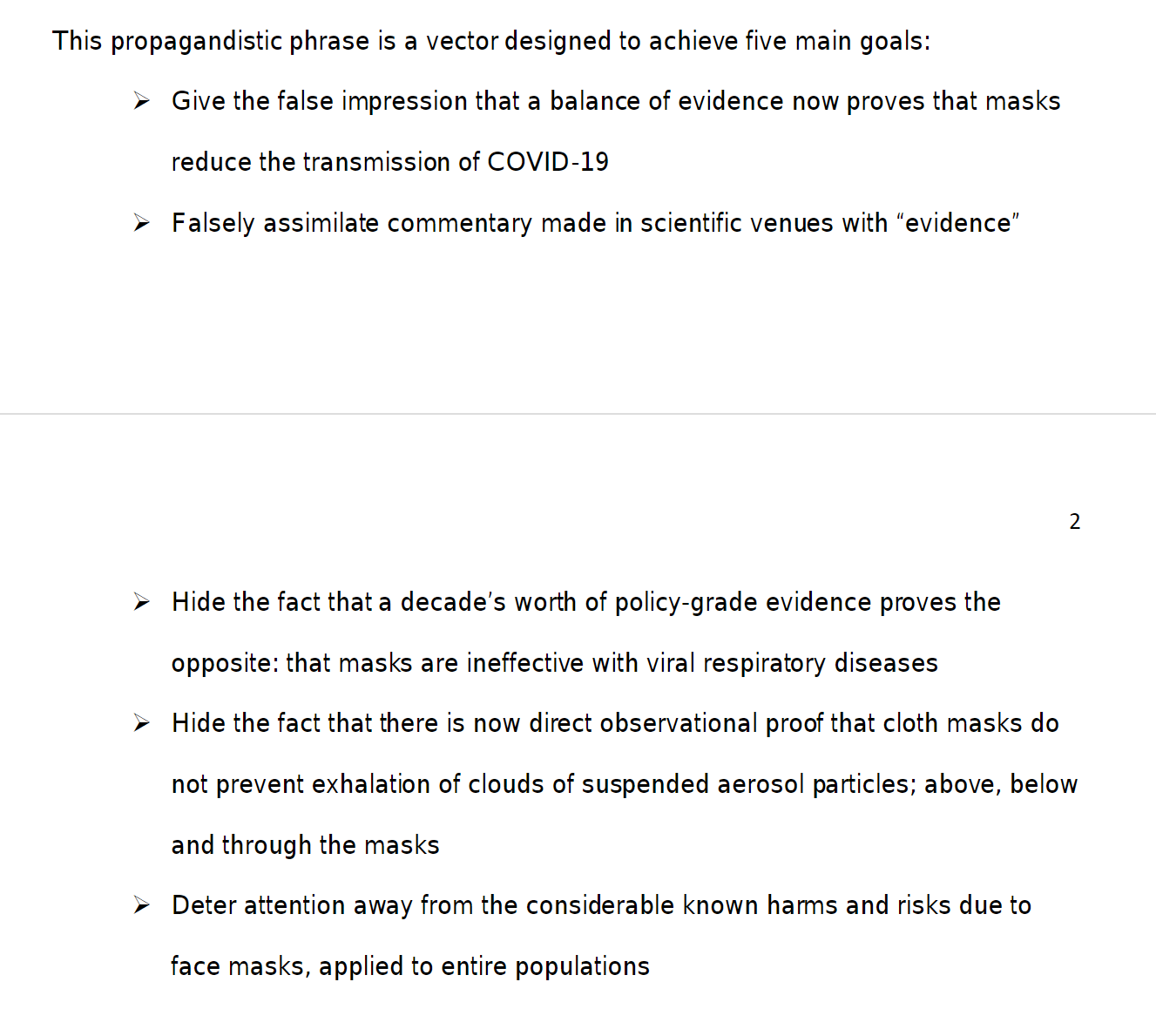
Lies, damned lies and public health officials
https://www.researchgate.net/publication/343399832_Face_masks_lies_damn_lies_and_public_health_officials_A_growing_body_of_evidence
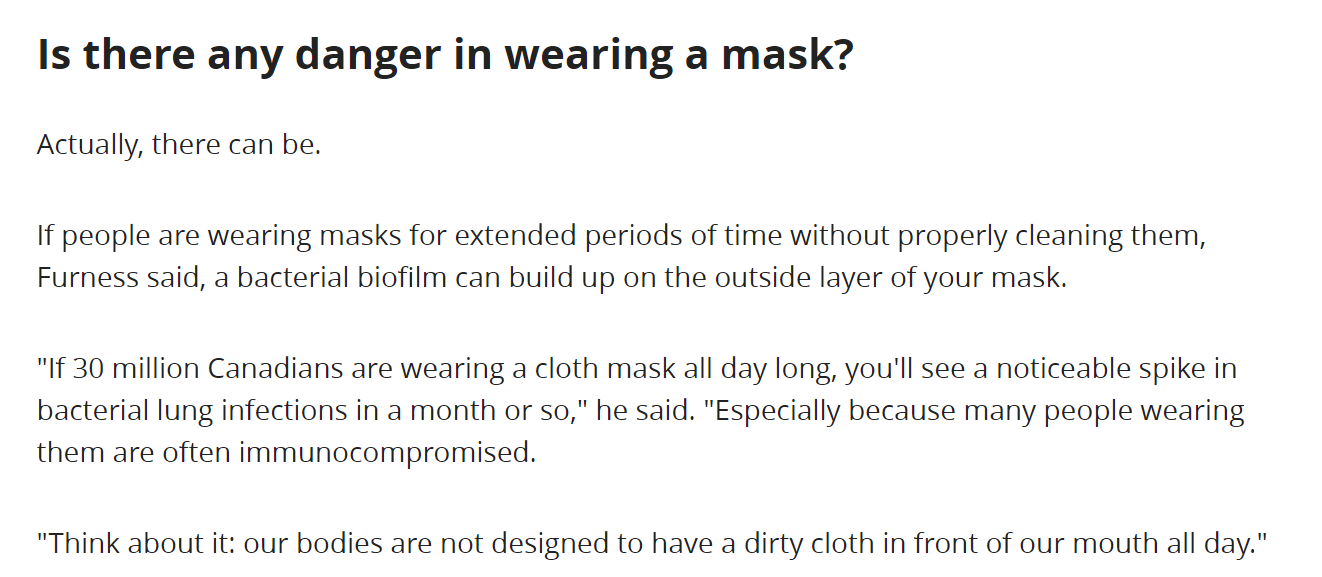
Dangers to wearing a mask:
https://www.cbc.ca/news/health/masks-covid-questions-answered-1.5580645
Union says can’t force nurses to wear masks
https://www.cbc.ca/news/canada/toronto/union-says-ontario-nurses-can-t-be-forced-to-wear-masks-in-flu-season-1.3222702
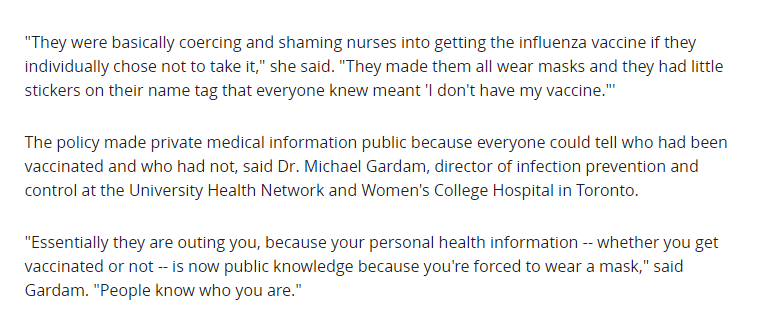
Nurses forced by hospital call in experts. Experts say “masks don’t work to reduce infection” and Nurses won 2 times.
1/ The Ontario arbitration fight about masks is really stunning. The background: several Ontario hospitals wanted to make all nurses get flu vaccinations. Legally they couldn’t. So they required the nurses who wouldn’t get vaccinated to wear masks. The nurses filed a grievance…
— Alex Berenson (@AlexBerenson) August 7, 2020
Still no conclusive evidence justifying mandatory masks
https://www.rcreader.com/commentary/still-no-conclusive-evidence-justifying-mandatory-masks#overlay-context=commentary/still-no-conclusive-evidence-justifying-mandatory-masks
Unsanitary and ineffective
https://12160.info/m/blogpost?id=2649739%3ABlogPost%3A2035264
CDC
https://wwwnc.cdc.gov/eid/article/26/5/19-0994_article
Masks Don’t Work
How long before the internet nukes this video? pic.twitter.com/oypngp8ZAi
— Justin Curley (@justcurl44) August 26, 2020
https://vixra.org/abs/2006.0044
Psychological impact of masking
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3879648/
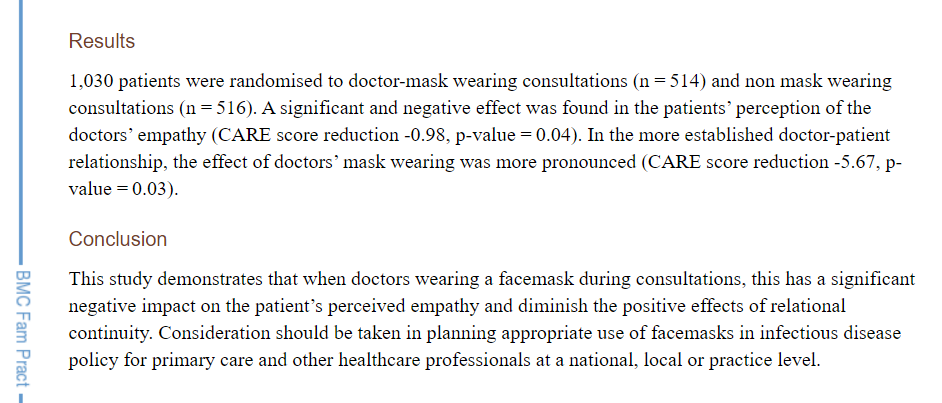
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3879648/
https://archive.is/mK9db#selection-1287.243-1287.552
E-MASK-ulation: How we have been lied to so dramatically about masks
Can anyone explain this? pic.twitter.com/b5glfJAQAe
— Ben (@BenMarten) September 9, 2020
Flu shots are a bad idea
https://doctormurray.com/does-the-flu-shot-increase-covid-19-risk/
https://www.disabledveterans.org/2020/03/11/flu-vaccine-increases-coronavirus-risk/
This is very interesting. Switzerland is divided into 26 provinces (cantons). Some cantons introduced mask mandates and others did not. Yet no difference in outcomes has been observed. https://t.co/06H4euiDMg
— Hans Mahncke (@HansMahncke) October 1, 2020
J Xiao, E Shiu, et al. Nonpharmaceutical measures for pandemic influenza in non-healthcare settings – personal protective and environmental measures. Centers for Disease Control. 26(5); 2020 May.
https://wwwnc.cdc.gov/eid/article/26/5/19-0994_article
J Brainard, N Jones, et al. Facemasks and similar barriers to prevent respiratory illness such as COVID19: A rapid systematic review. MedRxiv. 2020 Apr 1.
https://www.medrxiv.org/content/10.1101/2020.04.01.20049528v1.full.pdf
L Radonovich M Simberkoff, et al. N95 respirators vs medical masks for preventing influenza among health care personnel: a randomized clinic trial. JAMA. 2019 Sep 3. 322(9): 824-833.
https://jamanetwork.com/journals/jama/fullarticle/2749214
J Smith, C MacDougall. CMAJ. 2016 May 17. 188(8); 567-574.
https://www.cmaj.ca/content/188/8/567
F bin-Reza, V Lopez, et al. The use of masks and respirators to prevent transmission of influenza: a systematic review of the scientific evidence. 2012 Jul; 6(4): 257-267.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5779801/
J Jacobs, S Ohde, et al. Use of surgical face masks to reduce the incidence of the common cold among health care workers in Japan: a randomized controlled trial. Am J Infect Control. 2009 Jun; 37(5): 417-419.
https://pubmed.ncbi.nlm.nih.gov/19216002/
M Viola, B Peterson, et al. Face coverings, aerosol dispersion and mitigation of virus transmission risk.
https://arxiv.org/ftp/arxiv/papers/2005/2005.10720.pdf
S Grinshpun, H Haruta, et al. Performance of an N95 filtering facepiece particular respirator and a surgical mask during human breathing: two pathways for particle penetration. J Occup Env Hygiene. 2009; 6(10):593-603.
https://www.tandfonline.com/doi/pdf/10.1080/15459620903120086
F Blachere, W Lindsley et al. Assessment of influenza virus exposure and recovery from contaminated surgical masks and N95 respirators. J Viro Methods. 2018 Oct; 260:98-106.
https://pubmed.ncbi.nlm.nih.gov/30029810/
F Blachere, W Lindsley et al. Assessment of influenza virus exposure and recovery from contaminated surgical masks and N95 respirators. J Viro Methods. 2018 Oct; 260:98-106.
https://pubmed.ncbi.nlm.nih.gov/30029810/
A Chughtai, S Stelzer-Braid, et al. Contamination by respiratory viruses on our surface of medical masks used by hospital healthcare workers. BMC Infect Dis. 2019 Jun 3; 19(1): 91.
https://pubmed.ncbi.nlm.nih.gov/31159777/
L Zhiqing, C Yongyun, et al. J Orthop Translat. 2018 Jun 27; 14:57-62.
https://pubmed.ncbi.nlm.nih.gov/30035033/
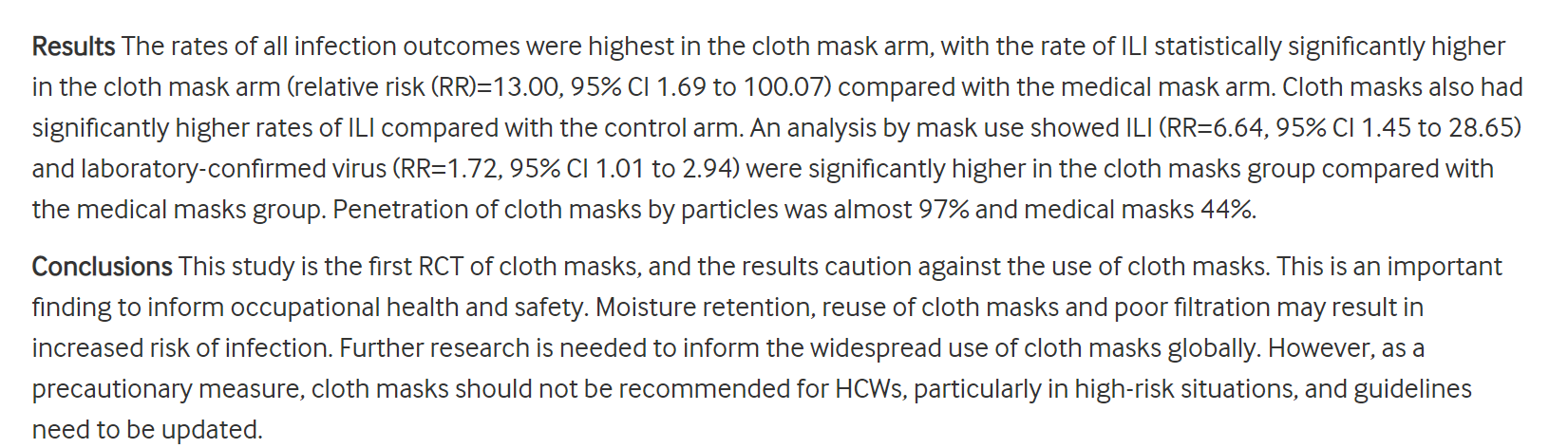
C MacIntyre, H Seale, et al. A cluster randomized trial of cloth masks compared with medical masks in healthcare workers. BMJ Open. 2015; 5(4)
https://bmjopen.bmj.com/content/5/4/e006577
A Beder, U Buyukkocak, et al. Preliminary report on surgical mask induced deoxygenation during major surgery. Neurocirugia. 2008; 19: 121-126.
http://scielo.isciii.es/pdf/neuro/v19n2/3.pdf
D Lukashev, B Klebanov, et al. Cutting edge: Hypoxia-inducible factor 1-alpha and its activation-inducible short isoform negatively regulate functions of CD4+ and CD8+ T lymphocytes. J Immunol. 2006 Oct 15; 177(8) 4962-4965.
https://www.jimmunol.org/content/177/8/4962
A Sant, A McMichael. Revealing the role of CD4+ T-cells in viral immunity. J Exper Med. 2012 Jun 30; 209(8):1391-1395.
https://europepmc.org/article/PMC/3420330
T Jefferson, M Jones, et al. Physical interventions to interrupt or reduce the spread of respiratory viruses. MedRxiv. 2020 Apr 7.
https://www.medrxiv.org/content/10.1101/2020.03.30.20047217v2
Bae, M Kim, et al. Effectiveness of surgical and cotton masks in blocking SARS-CoV-2: A controlled comparison in 4 patients. Ann Int Med. 2020 Apr 6.
https://www.acpjournals.org/doi/10.7326/M20-1342
S Rengasamy, B Eimer, et al. Simple respiratory protection – evaluation of the filtration performance of cloth masks and common fabric materials against 20-1000 nm size particles. Ann Occup Hyg. 2010 Oct; 54(7): 789-798.
https://academic.oup.com/annweh/article/54/7/789/202744
C MacIntyre, H Seale, et al. A cluster randomized trial of cloth masks compared with medical masks in healthcare workers. BMJ Open. 2015; 5(4)
https://bmjopen.bmj.com/content/5/4/e006577.long
W Kellogg. An experimental study of the efficacy of gauze face masks. Am J Pub Health. 1920. 34-42.
https://ajph.aphapublications.org/doi/pdf/10.2105/AJPH.10.1.34
M Klompas, C Morris, et al. Universal masking in hospitals in the Covid-19 era. N Eng J Med. 2020; 382 e63.
https://www.nejm.org/doi/full/10.1056/NEJMp2006372
E Person, C Lemercier et al. Effect of a surgical mask on six minute walking distance. Rev Mal Respir. 2018 Mar; 35(3):264-268.
https://pubmed.ncbi.nlm.nih.gov/29395560/
B Chandrasekaran, S Fernandes. Exercise with facemask; are we handling a devil’s sword – a physiological hypothesis. Med Hypothese. 2020 Jun 22. 144:110002.
https://pubmed.ncbi.nlm.nih.gov/32590322/
P Shuang Ye Tong, A Sugam Kale, et al. Respiratory consequences of N95-type mask usage in pregnant healthcare workers – A controlled clinical study. Antimicrob Resist Infect Control. 2015 Nov 16; 4:48.
https://pubmed.ncbi.nlm.nih.gov/26579222/
T Kao, K Huang, et al. The physiological impact of wearing an N95 mask during hemodialysis as a precaution against SARS in patients with end-stage renal disease. J Formos Med Assoc. 2004 Aug; 103(8):624-628.
https://pubmed.ncbi.nlm.nih.gov/15340662/
Lopp & Edwards reviewed the surgical literature in 2014 and found “no statistically significant difference in infection rates between the masked and unmasked group in any of the trials.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD002929.pub2/full
In a 2014 review based on four studies and 6,006 patients, wrote that “none of the four studies found a difference in the number of post-operative infections whether you used a surgical mask or not.
https://europepmc.org/article/med/25294675
Salassa and Swiontkowski, in 2014, investigated the necessity of scrubs, masks and head coverings in the operating room and concluded that “there is no evidence that these measures reduce the prevalence of surgical site infection
https://journals.lww.com/jbjsjournal/Abstract/2014/09030/Surgical_Attire_and_the_Operating_Room__Role_in.11.aspx
Da Zhou et al., reviewing the literature in 2015, concluded that “there is a lack of substantial evidence to support claims that facemasks protect either patient or surgeon from infectious contamination
https://journals.sagepub.com/doi/pdf/10.1177/0141076815583167
L Brosseau, M Sietsema. Commentary: Masks for all for Covid-19 not based on sound data. U Minn Ctr Inf Dis Res Pol. 2020 Apr 1.
https://www.cidrap.umn.edu/news-perspective/2020/04/commentary-masks-all-covid-19-not-based-sound-data
N Leung, D Chu, et al. Respiratory virus shedding in exhaled breath and efficacy of face masks Nature Research. 2020 Mar 7. 26,676-680 (2020).
https://www.researchsquare.com/article/rs-16836/v1
S Rengasamy, B Eimer, et al. Simple respiratory protection – evaluation of the filtration performance of cloth masks and common fabric materials against 20-1000 nm size particles. Ann Occup Hyg. 2010 Oct; 54(7): 789-798.
https://academic.oup.com/annweh/article/54/7/789/202744
Lahme et al.,in 2001, wrote that “surgical face masks worn by patients during regional anaesthesia, did not reduce the concentration of airborne bacteria over the operation field in our study. Thus they are dispensable
https://europepmc.org/article/med/11760479
Figueiredo et al. in 2001, reported that in five years of doing peritoneal dialysis without masks, rates of peritonitis in their unit were no different than rates in hospitals where masks were worn
http://www.advancesinpd.com/adv01/21Figueiredo.htm
Bahli did a systematic literature review in 2009 and found that “no significant difference in the incidence ofpostoperative wound infection was observed between masks groups and groups operated with no masks
https://pdfs.semanticscholar.org/751a/cd427c20c8dc7d1fbc1b45eead104286f481.pdf
Bahli in Sweden, recognizing the lack of evidence supporting the use of masks, ceased requiring them in 2010 for anesthesiologists and other non-scrubbed personnel in the operating room. “Our decision to no longer require routine surgical masks for personnel not scrubbed for surgery is a departure from common practice. But the evidence to support this practice does not exist,” wrote Dr. Eva Sellden.
https://pubs.asahq.org/anesthesiology/article/113/6/1447/9572/Is-Routine-Use-of-a-Face-Mask-Necessary-in-the
Surgeons at the Karolinska Institutein 2010, reported on obstetric, gynecological, general, orthopaedic, breast and urological surgeries performed on 827 patients. All non-scrubbed staff wore masks in half the surgeries, and none of the non-scrubbed staff wore masks in half the surgeries. Surgical site infections occurred in 11.5% of the Mask group, and in only 9.0% of the No Mask group.
https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1445-2197.2009.05200.x
Ritter et al in 1975, found that “the wearing of a surgical face mask had no effect upon the overall operating room environmental contamination.
https://pubmed.ncbi.nlm.nih.gov/1157412/
Ha’eri and Wiley in 1980, applied human albumin microspheres to the interior of surgical masks in 20 operations. At the end of each operation, wound washings were examined under microscope. “Particle contamination of the wound was demonstrated in all experiments.”
https://europepmc.org/article/med/7379387
Laslett and Sabin, in 1989, found that caps and masks were not necessary during cardiac catheterization. “No infections were found in any patient, regardless of whether a cap or mask was used
https://onlinelibrary.wiley.com/doi/abs/10.1002/ccd.1810170306
In Tunevall’s 1991 study,a general surgical team wore no masks in half of their surgeries for two years. After 1,537 operations performed with masks, the wound infection rate was 4.7%, while after 1,551 operations performed without masks, the wound infection rate was only 3.5%
https://link.springer.com/article/10.1007/BF01658736
A review by Skinner and Sutton in 2001 concluded that “The evidence for discontinuing the use of surgical face masks would appear to be stronger than the evidence available to support their continued use
https://journals.sagepub.com/doi/pdf/10.1177/0310057X0102900402